Print | Back to Main Guidelines Listing
Northern California Neonatal Consortium
This work is licensed under a Creative Commons Attribution-Noncommercial 4.0 International License
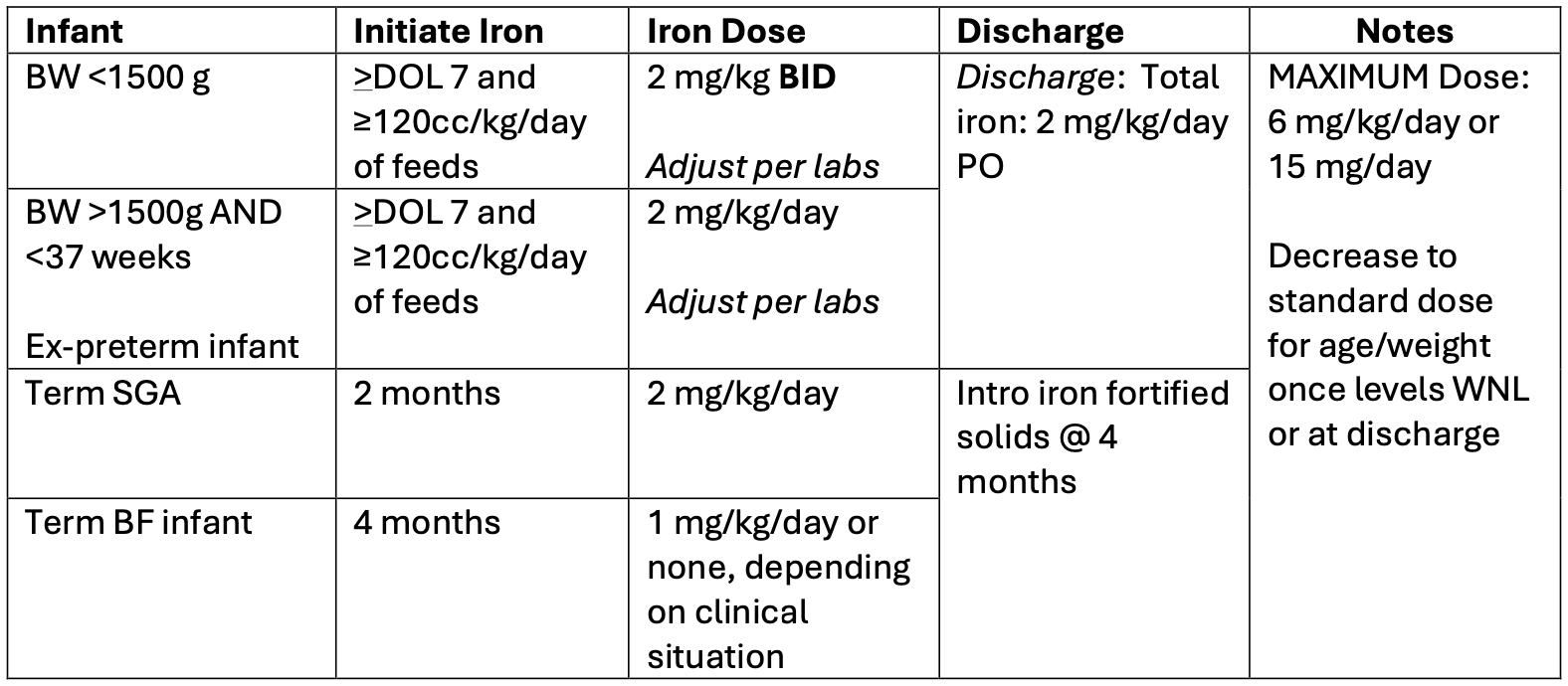
Iron Supplementation Guidelines
Enteral Iron Supplementation
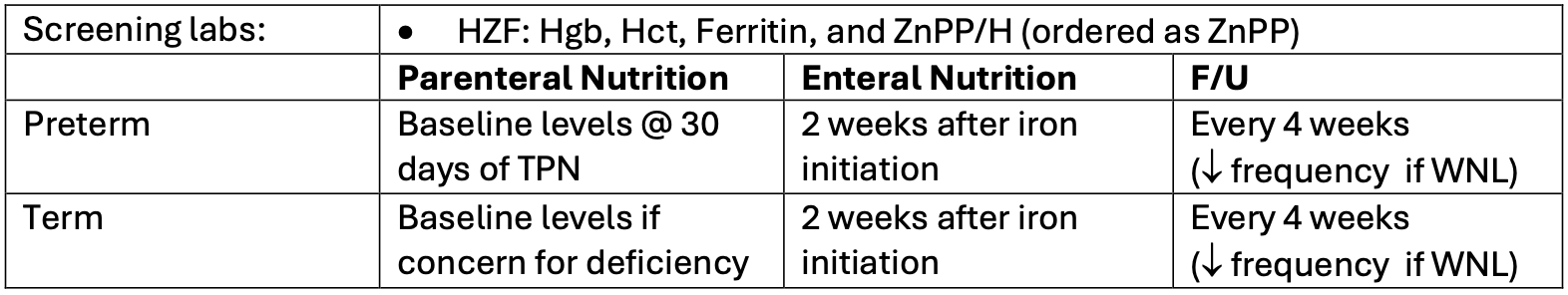
Monitoring and Screening Labs:
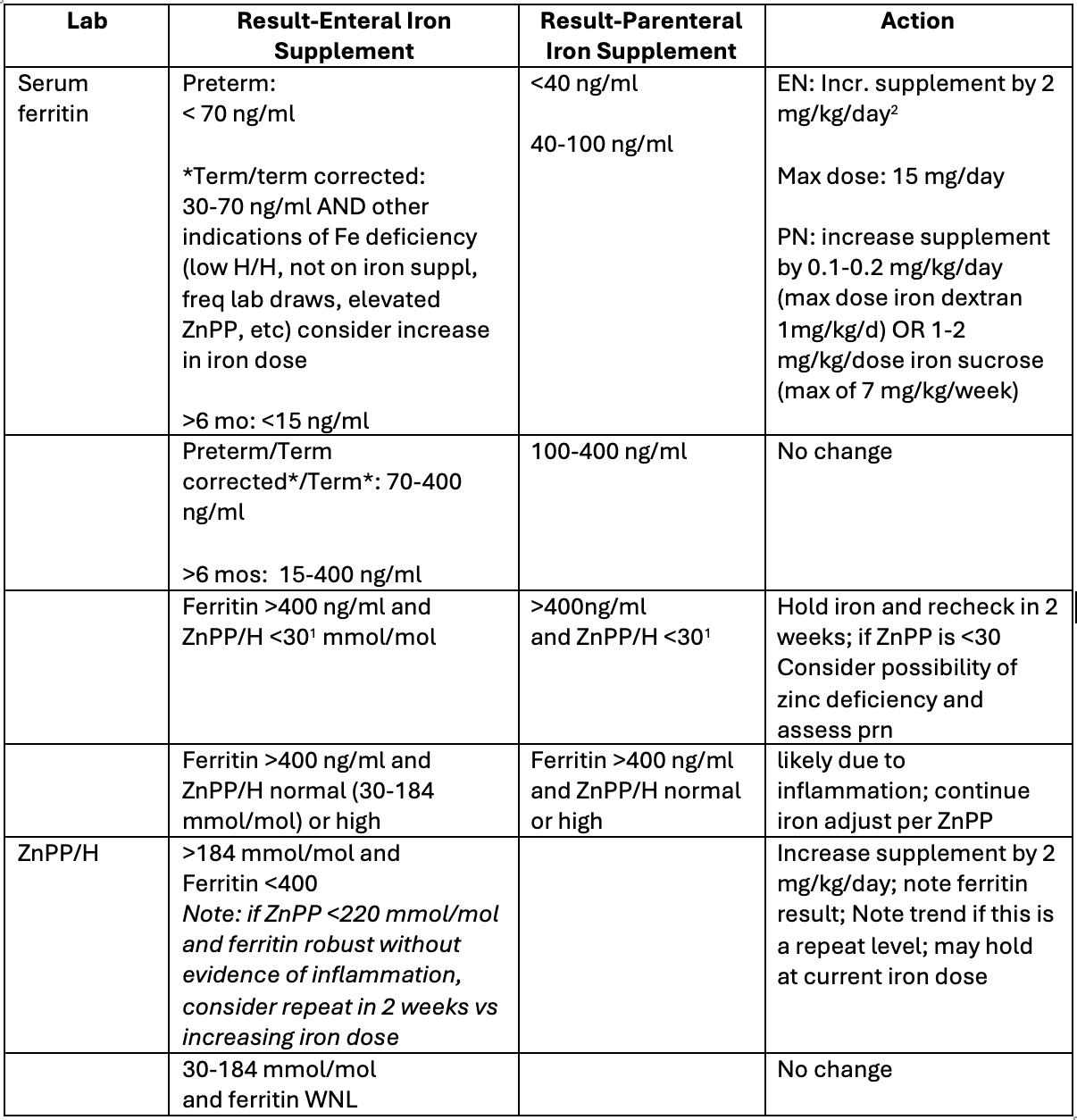
Results:
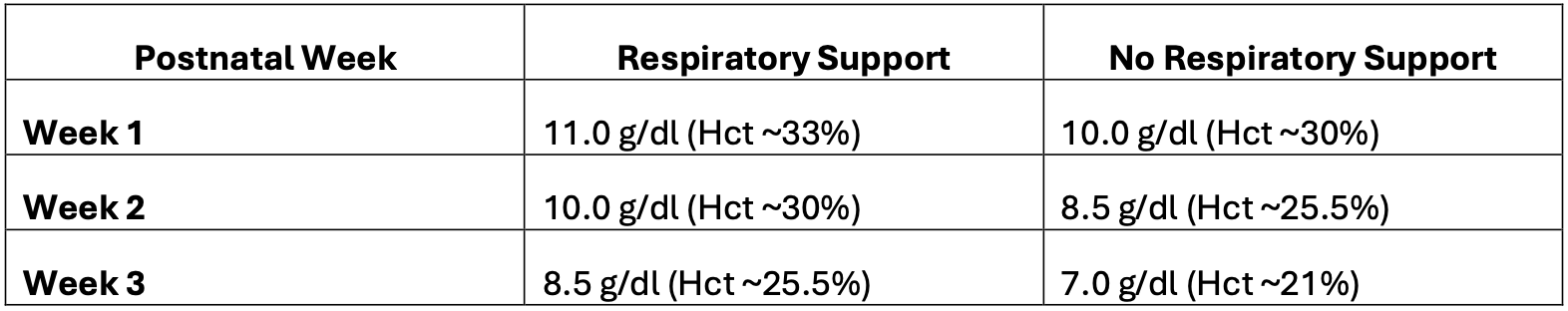
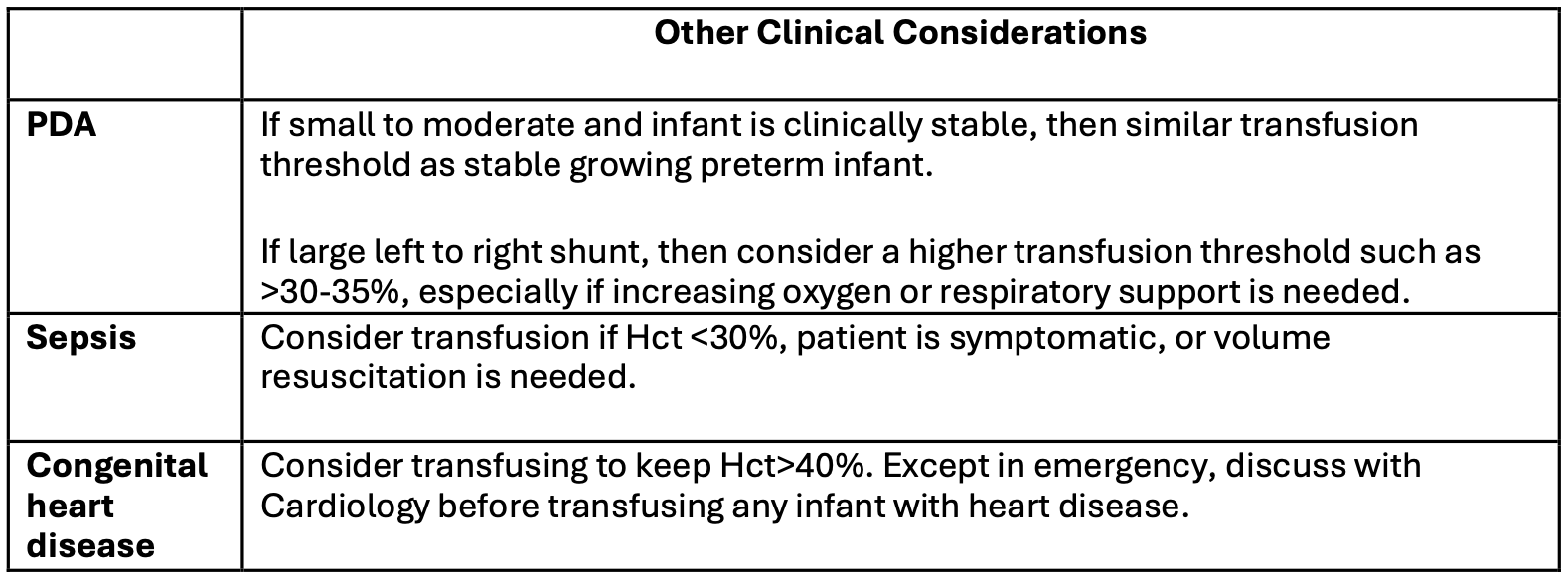
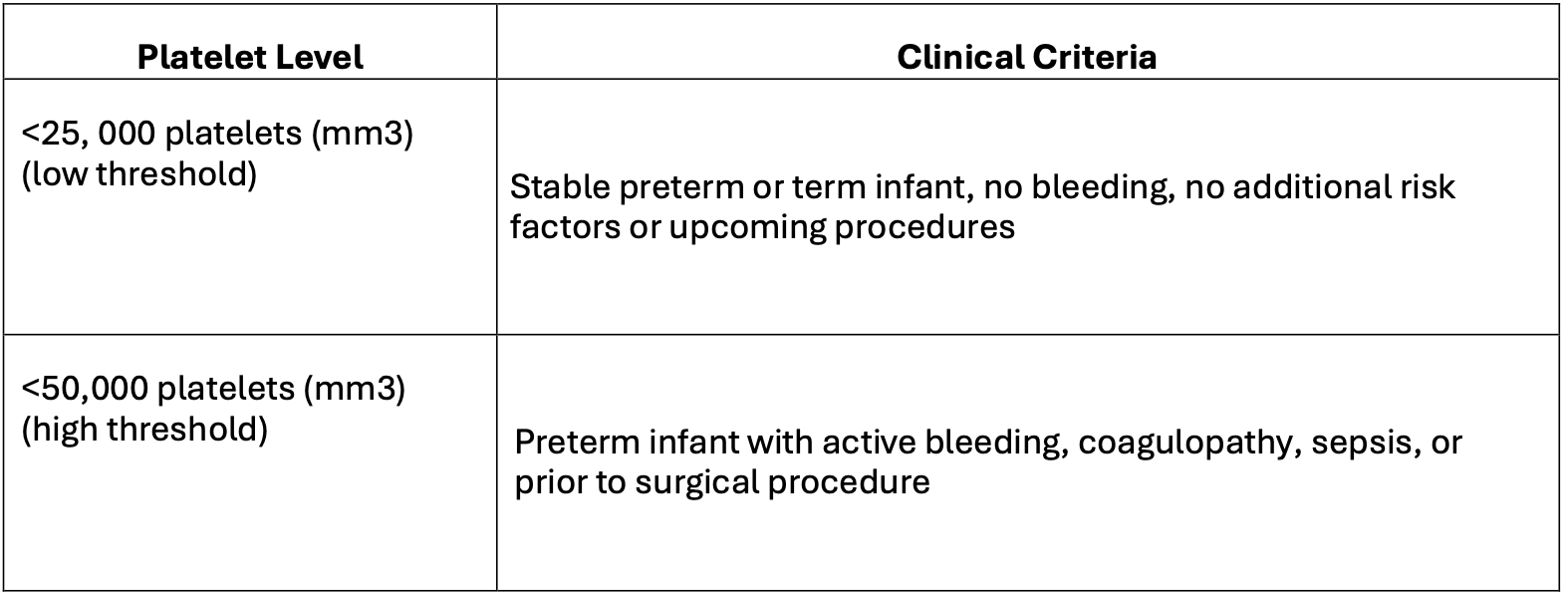
Transfusion Guidelines
Hemoglobin thresholds for transfusion of Packed Red Blood Cells (pRBCs):
Platelets threshold for transfusion:
References:
- Barbieri J and Cober MP. Select micronutrients for the preterm neonate Nutr. Clin. Pract. 2023;38:S66–S83.
- Chan KC e al. Iron status of full-term infants in early infancy is not associated with maternal ferritin levels nor infant feeding practice British Journal of Nutrition (2022), 127, 1198–1203
- Cheng et al. ZnPP/heme in high risk preterm infants J Pediatr2012;16(1):81-7.
- De Waal, CG et. Zinc protoporphyrin/heme ratio as parameter of iron status in moderately preterm infants: natural course and associations in the first 4 months J Perinatology 2017;(37):690–694
- Domellf, M. ESPGHAN Committee of Nutrition (CoN) position paper on Enteral Nutrition for Preterm Infants 2022 Trace elements; February 2022
- German KR et al. ZPP and Ferritin as Measures of Iron Sufficiency in the NICU J Pediatr 2018;194:47-53
- German, KR et al. Enteral Iron Supplementation in Infants Born Extremely Preterm and its Positive Correlation with Neurodevelopment; Post Hoc Analysis of the Preterm Erythropoietin Neuroprotection Trial Randomized Controlled Trial J Pediatr 2021;238:102-9.
- Kirpalani H, etal. Enteral Iron Supplementation in Preterm or Low Birth Weight Infants: A Systematic Review and Meta-analysis. Pediatrics. 2022
- Juul SE et al. ZnPP/Heme as an Indicator of Iron Status in NICU Paatients J Pediatr 2003;142:273-8
- McCarthy EK et al. Iron supplementation in preterm and low-birth-weight infants: a systematic review of intervention studies. Nutr Rev. 2019.
- Raghavendra R et al, Iron Therapy for preterm Infants. Clin Perinatol. 2009 March ; 36(1): 27–42. doi:10.1016/j.clp.2008.09.013
- Kirpalani H, Bell EF, Hintz SR, et al; Eunice Kennedy Shriver NICHD Neonatal Research Network. Higher or lower hemoglobin transfusion thresholds for preterm infants. N Engl J Med. 2020;383(27):2639-2651 doi:10.1056/NEJMoa2020248
- Deschmann E, Dame C, Sola-Visner MC, et al. Clinical Practice Guideline for Red Blood Cell Transfusion Thresholds in Very Preterm Neonates. JAMA Netw Open. 2024;7(6):e2417431. doi:10.1001/jamanetworkopen.2024.17431
- Curley A, Stanworth SJ, Willoughby K, Fustolo-Gunnink SF, Venkatesh V, Hudson C, Deary A, Hodge R, Hopkins V, Lopez Santamaria B, Mora A, Llewelyn C, D'Amore A, Khan R, Onland W, Lopriore E, Fijnvandraat K, New H, Clarke P, Watts T; PlaNeT2 MATISSE Collaborators. Randomized Trial of Platelet-Transfusion Thresholds in Neonates. N Engl J Med. 2019 Jan 17;380(3):242-251. doi: 10.1056/NEJMoa1807320. Epub 2018 Nov 2. PMID:30387697.
- Test Catalog - Mayo Clinic Laboratories (mayocliniclabs.com)
- UCSF Clinical Laboratories Test Directory | Home (testmenu.com)
Disclaimer
These clinical practice guidelines are based upon the evidence-based consensus opinions of consortium members affiliated with UCSF Benioff Children's Hospitals. They are intended to guide pediatric/neonatal providers, but do not substitute for individual clinical judgment. Evaluation and treatment of specific patients should be adapted based upon the unique conditions of each patient, family and clinical environment.
UCSF Multi-Site Neonatology Collaboration. Originated 06/2025
Approved by UCSF Pharmacy and Therapeutics Committee: 6/2025



